
Flexibility and adaptability should be key design considerations as the paradigm constantly shifts. Once standard waiting rooms, workstations and exam rooms are now evolving to accommodate new delivery models and a highly diverse patient-base. Informed medical planning can identify these changes and evaluate specific needs to find the ideal clinical configurations for healthcare providers. The key to finding the right option for you lies in understanding your unique demographics, identifying the types of services and care model you want to provide, and standardizing your facility where possible.
Typical clinical configurations
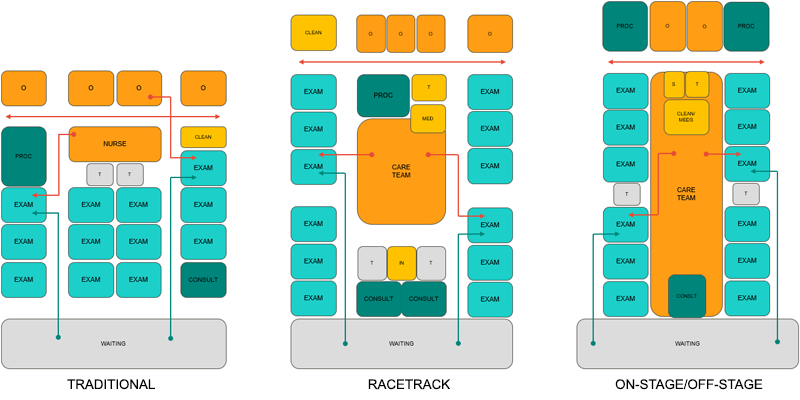
TRADITIONAL MODEL
In this model, each provider has their own pod, complete with a private office and dedicated exam rooms. The support space is remote while public and staff share the same corridors.
RACETRACK MODEL
Each provider has dedicated exam rooms and support is both internal and external facing. Public and staff corridors are semi-split and the layout accommodates multiple service lines.
ON-STAGE/OFF-STAGE MODEL
Each provider has dedicated exam rooms, but their office is remote. The support space is internal, allowing a team of caregivers to collaborate together for coordinated care. Two exam room doors provide separate access from public and staff corridors.
Which configuration is right for you?
Informed medical planning makes selecting a clinical model easy. To reach a decision on general configuration and layout that you can be confident in, start with these questions:
- How long do your patients wait to be submitted to an exam or consult room when they arrive at your clinic?
- How many steps do your patients travel to an exam or consult room?
- Do your patients have to change rooms while they are visiting your clinic?
- What consultation or multipurpose spaces do providers need to discuss preventative care resources?
- Where are procedure rooms located and how many do you have?
- Is the physician working with medical assistants and support staff inside a collaborative care team zone?
- Is a separate sit-down nurse area needed for each provider?
- Do you and your patients have the ability to connect virtually?
- How are supplies distributed?
Once a clinical model is selected, you can begin more detailed discussions to refine the design. Start with questions such as:
- How do care team members communicate with the patients and families?
- Is there enough space for care team members to visit the patient and share records or patient information while maintaining face-to-face contact with the patient?
- How important are larger family spaces in exam rooms to accommodate family, friends or interpreters?
- What patient and family accommodations are needed? (i.e. number of chairs, benches, magazines racks, pamphlet displays, coat hooks, etc.)
- How would a swinging door and sliding door make a difference for you?
- What current and forward-thinking technology is needed? (i.e. video-based telemedicine that allows patients and providers to consult with specialists remotely, or technology to support self-check-in and rooming)
- What supplies are needed in every exam room?
With so many changes happening inside the clinic environment, forward-thinking medical planners need to collaborate with their clients to review the best options in the evolving marketplace. Efficient, well-planned clinics anticipate changes to provide the best patient care possible.